"Normal" Test Results, But Still Feel Unwell? Here is What to Do Next
- Dr Hassan Paraiso
- Dec 3, 2025
- 5 min read
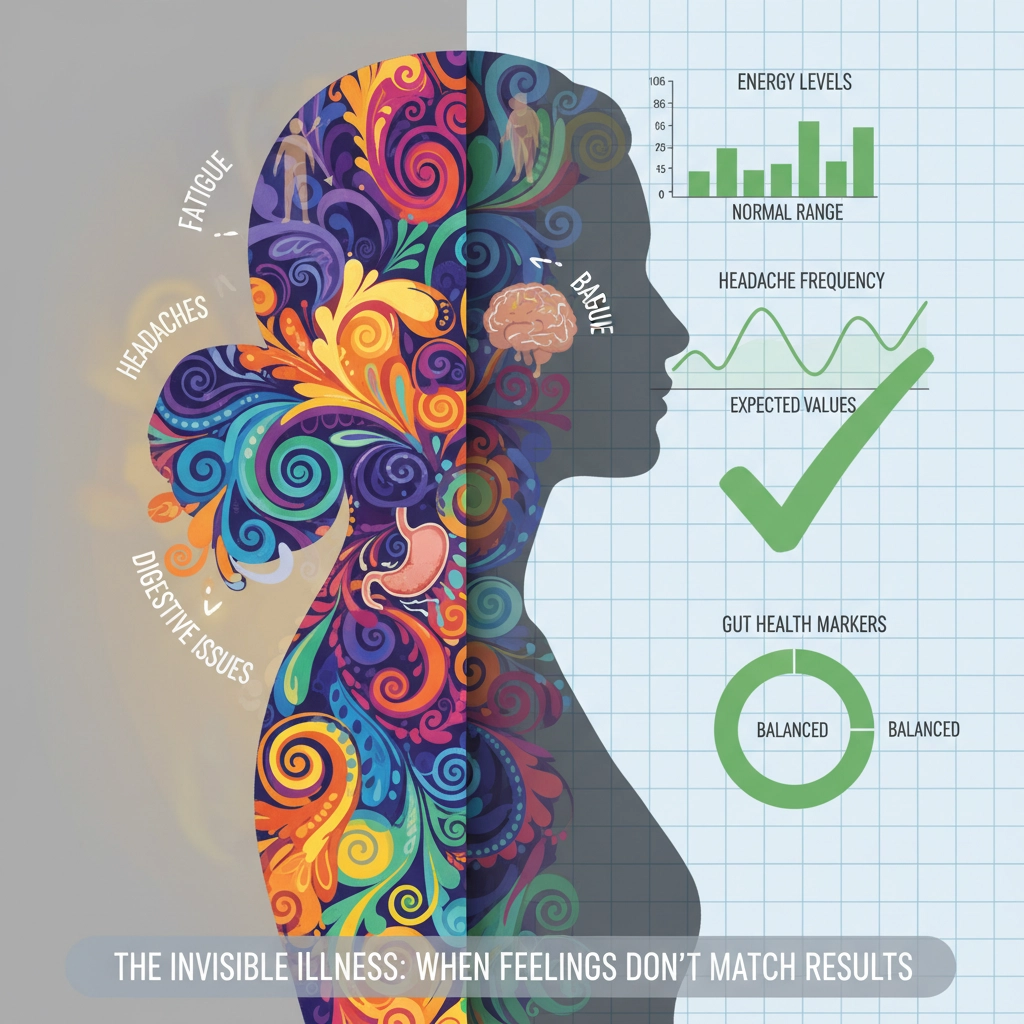
It's one of the most frustrating experiences in healthcare: you're feeling genuinely unwell, you've undergone tests, and everything comes back "normal." Yet you still feel terrible. You're not imagining it, and you're certainly not alone. This scenario happens far more frequently than many people realise, and there are clear, practical steps you can take to get the answers and care you deserve.
Why "Normal" Test Results Don't Always Mean You're Well
The fundamental issue lies in how we interpret medical testing. When a doctor says your results are "normal," they typically mean your values fall within the standard reference ranges used by laboratories. However, these ranges are often quite broad, and what's considered "normal" for the general population might not be optimal for you as an individual.
Reference ranges are usually established by testing large groups of people and setting the "normal" range to include about 95% of results. This means that 5% of healthy people will always fall outside the normal range, and conversely, you can feel unwell while still falling within it. Your thyroid function might be at the bottom end of normal, your vitamin levels might be adequate but not optimal, or you might have subtle abnormalities that standard tests simply don't detect.

Additionally, many conditions don't show up on routine blood tests at all. Chronic fatigue syndrome, fibromyalgia, certain autoimmune conditions in their early stages, and various neurological issues may not produce clearly abnormal laboratory results, despite causing significant symptoms.
The Value of Consultant Review
This is where specialist medical expertise becomes invaluable. While initial testing through standard pathways serves an important role, consultant physicians bring a different level of analytical depth to complex cases. A consultant can interpret your results within the broader context of your symptoms, medical history, and individual circumstances.
Consultants are trained to recognise patterns that might not be immediately obvious and to consider diagnoses that require more sophisticated investigation. They can identify when "normal" results actually represent meaningful trends or when additional, more specialised testing might be warranted. Most importantly, they can coordinate a comprehensive approach to your care rather than examining isolated symptoms or test results.
Document Your Symptoms Systematically
While you're seeking specialist input, start creating a detailed symptom diary. This isn't just busy work – it's one of the most powerful diagnostic tools available. Record not just what you're experiencing, but when symptoms occur, how long they last, what triggers them, and what provides relief.
Include details about your energy levels throughout the day, sleep quality, any digestive issues, mood changes, and physical symptoms. Note any patterns related to food, stress, weather, or activity levels. This comprehensive picture often reveals connections that isolated test results simply cannot capture.
Present this information clearly and concisely – ideally as a one-page summary that highlights the most significant patterns. This focused approach helps consultants quickly identify potential diagnoses they might otherwise overlook and demonstrates that you're an engaged partner in solving your health puzzle.
Consider Targeted Additional Testing
Depending on your symptoms, more specialised investigations might provide crucial insights that standard panels miss. A comprehensive thyroid assessment, for example, goes beyond basic TSH testing to include T3, T4, reverse T3, and thyroid antibodies. Vitamin D levels, B12 with methylmalonic acid, comprehensive mineral panels, and inflammatory markers can all reveal deficiencies or imbalances that explain persistent symptoms.
Some consultants may recommend functional medicine approaches that examine gut health through comprehensive stool analysis, assess stress response through salivary cortisol patterns, or investigate food sensitivities through elimination protocols. While not all additional testing is necessary or beneficial, the right tests ordered by an experienced consultant can provide breakthrough insights.
The Importance of Joined-Up Care
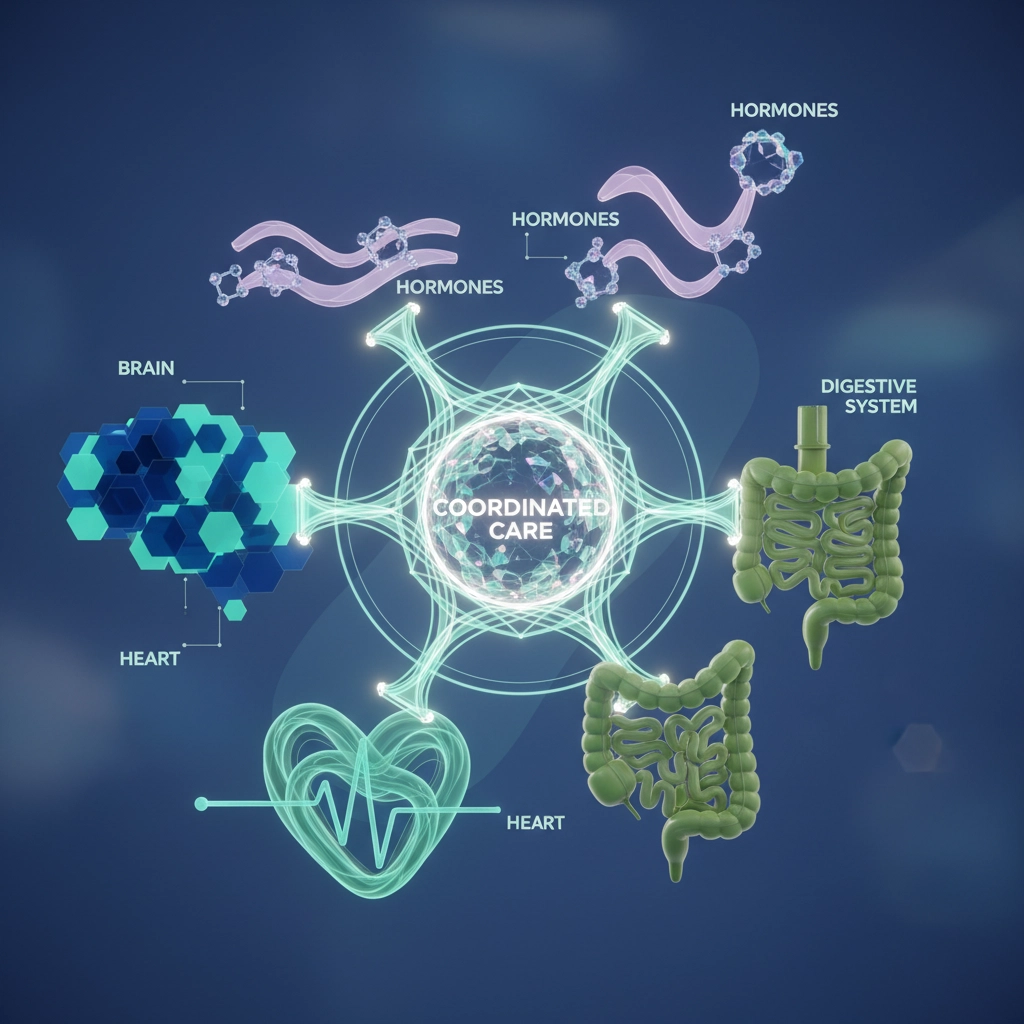
One of the significant advantages of consultant-led care is the coordination it provides. Rather than bouncing between different specialists who each examine one aspect of your health, a consultant physician can oversee your entire case, ensuring that all the pieces of your health puzzle are considered together.
This joined-up approach is particularly valuable when dealing with complex, multi-system symptoms. Your fatigue might be related to sleep issues, which connect to hormonal imbalances, which link to nutritional deficiencies – connections that become clear only when someone is looking at the complete picture.

Consultants also have established relationships with other specialists. They can facilitate efficient referrals when needed, ensuring you receive the right expertise at the right time without unnecessary delays or duplicated testing.
Practical Steps You Can Take Now
While pursuing specialist input, there are evidence-based steps you can implement immediately. Prioritise sleep hygiene – aim for consistent sleep and wake times, create a restful environment, and address any obvious sleep disruptors. Chronic sleep deprivation can mimic or exacerbate numerous medical conditions.
Evaluate your stress management. Chronic stress affects virtually every body system and can maintain symptoms even after underlying issues are addressed. Consider whether stress reduction techniques, whether through mindfulness, exercise, or lifestyle modifications, might benefit your overall health.
Examine your diet critically. Food sensitivities, blood sugar fluctuations, and nutritional deficiencies are commonly overlooked causes of persistent symptoms. A whole food diet that minimises processed foods and sugar often provides improvements even before specific diagnoses are confirmed.
When to Stop Testing and Focus on Recovery
There's an important balance between thorough investigation and excessive testing. Additional tests should be targeted and purposeful rather than exhaustive. Once you've had appropriate evaluation of the most likely causes of your symptoms, the focus may need to shift from continued testing to active management and recovery.
A skilled consultant will help you navigate this decision, ensuring you've had adequate investigation without falling into the trap of endless testing that may produce false positives, increase anxiety, or delay effective treatment.
Moving Forward Effectively
Remember that feeling unwell despite normal test results doesn't mean you're "fine" – it means you need a more sophisticated approach to your healthcare. The combination of detailed symptom documentation, consultant-level expertise, and targeted additional testing when appropriate often provides the answers that initial investigations missed.
Your symptoms are real, your concerns are valid, and solutions are available. The key is working with healthcare providers who understand that optimal health extends beyond simply avoiding clearly abnormal test results. With patience, thorough investigation, and expert guidance, most people in this situation do find explanations for their symptoms and effective paths to recovery.
The goal isn't just to rule out serious conditions – though that's important – but to optimise your health and quality of life. This requires a consultant who sees beyond individual test results to understand you as a complete person, with unique health needs and goals.
Health worries can grow quickly—especially when searching online—but a focused review often brings clarity. My role is to help you step out of the cycle of uncertainty and into a practical, balanced plan. If you feel an expert opinion would help, you’re welcome to arrange a private consultation at the clinic.


Comments