Chronic Fatigue With 'Normal Bloods': 10 Things Your GP Couldn't Check in a 10-Minute Slot
- Dr Hassan Paraiso
- 3 days ago
- 6 min read
"Everything came back normal." It's the phrase that brings both relief and frustration in equal measure when you're exhausted, struggling to function, and certain that something is wrong. You've done the blood tests, answered the questions, and still, you're no closer to understanding why you can barely get through the day.
Here's what I need you to understand first: normal blood tests are genuinely good news. They've ruled out some important things. But they're also a starting point, not the finish line. And in a 10-minute GP appointment, which is what most surgeries offer, there simply isn't time to explore the dozens of other possible causes of persistent fatigue.
This isn't a criticism of GPs. They're managing impossible workloads with skill and care. But when fatigue has no obvious cause, it often needs more time, a broader lens, and sometimes specialist investigations that standard NHS bloods don't include.
Let's talk about what might have been missed.

1. Postural orthostatic tachycardia syndrome (PoTS)
PoTS is a disorder of the autonomic nervous system that causes dizziness, palpitations, and overwhelming fatigue, especially on standing. It won't show up on routine bloods because it's a problem with how your body regulates heart rate and blood pressure, not with your blood itself.
Diagnosis requires specific tests: lying and standing blood pressure measurements over several minutes, heart rate monitoring, and sometimes a tilt-table test. These aren't part of a standard GP appointment, and many GPs aren't familiar with PoTS because it's relatively uncommon.
2. Sleep apnoea and other sleep disorders
You might think you sleep fine, but obstructive sleep apnoea (OSA) can cause profound daytime fatigue without you realising your breathing stops repeatedly through the night. Partners sometimes notice snoring or gasping, but not always.
Screening requires an overnight sleep study, either at home or in a specialist centre, which records oxygen levels, breathing patterns, and sleep stages. A blood test won't detect it. If you're over 50, male, overweight, or have a large neck circumference, OSA becomes statistically more likely and warrants proper investigation.
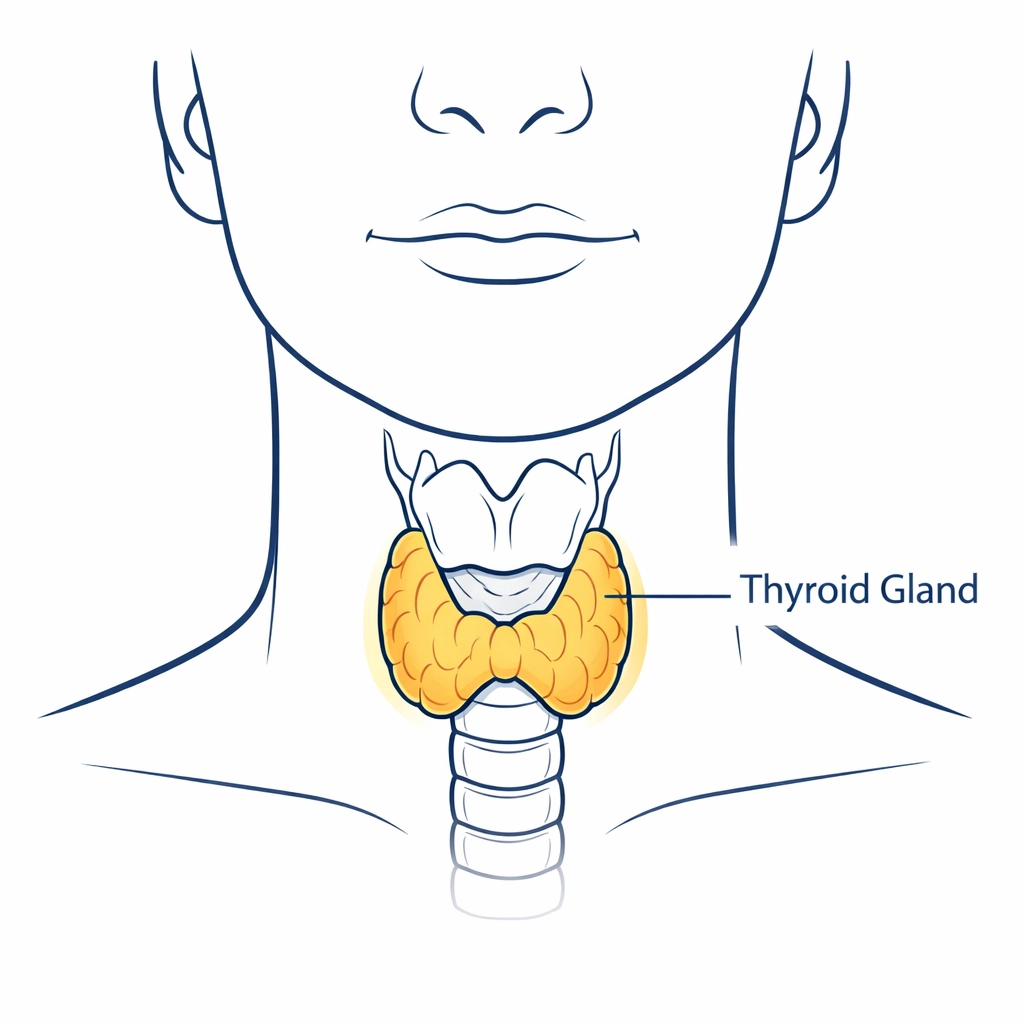
3. Suboptimal thyroid function within the 'normal' range
Your thyroid function test might say "normal," but normal is a range, not a single number. Some people feel dreadful with a TSH at the upper end of normal (say, 4.5 mIU/L), even though it's technically fine.
More detailed thyroid assessment, looking at free T3, free T4, thyroid antibodies (for autoimmune thyroid disease), and considering symptoms alongside numbers, takes time and expertise. In a 10-minute slot, if your TSH is within range, the conversation often stops there.
4. Vitamin and mineral deficiencies beyond the basics
Most GPs will check vitamin B12, folate, and ferritin (iron stores). But fatigue can also stem from low vitamin D, magnesium, or zinc, none of which are routinely tested.
Even when ferritin is checked, a result of 30 µg/L might be labelled "normal" (the lab reference range often starts around 15), but many people, especially women, feel significantly better once ferritin is above 50 or even 70. Optimising levels, not just avoiding deficiency, sometimes makes all the difference.
5. Coeliac disease (if you haven't been tested properly)
Fatigue is a common but underappreciated symptom of coeliac disease, which is an autoimmune reaction to gluten. Many people with coeliac disease don't have obvious gut symptoms.
The blood test (tissue transglutaminase antibodies, or tTG-IgA) is simple, but you must be eating gluten regularly for it to be accurate. If you've already cut out bread and pasta because you "feel better without them," the test might be falsely negative. And if your IgA levels are low (which some people have), you need a different test altogether, IgG-based coeliac serology.

6. Chronic infections: Epstein-Barr virus, Lyme, and others
Post-viral fatigue is real and can linger for months after infections like glandular fever (Epstein-Barr virus) or COVID-19. But standard GP bloods don't routinely check for these unless you mention a specific trigger.
Lyme disease, transmitted by ticks, can cause relapsing fatigue, joint pain, and neurological symptoms, but the NHS blood test for Lyme isn't always sensitive in early disease. If there's a possibility of tick exposure (countryside walks, camping, even parks in some parts of the UK), it's worth discussing.
7. Adrenal insufficiency (not just Addison's disease)
Addison's disease, complete adrenal failure, is rare and usually picked up because people become very unwell. But subtler forms of adrenal dysfunction can cause fatigue, low blood pressure, dizziness, and salt cravings.
Testing involves a morning cortisol level (which is sometimes checked) and, if borderline, a synacthen stimulation test to see how well your adrenals respond to stress. This requires hospital attendance and takes a couple of hours. It's not something a GP can arrange casually within a 10-minute consultation.
8. Autonomic dysfunction and chronic fatigue syndrome (ME/CFS)
ME/CFS is a diagnosis of exclusion, meaning it's only made after other causes have been ruled out. It's characterised by profound fatigue that worsens after physical or mental exertion (known as post-exertional malaise), sleep disturbances, and cognitive difficulties.
Recent research has identified specific immune cell and DNA folding abnormalities in ME/CFS patients, but these tests aren't available in routine NHS practice, they're research-level investigations. Diagnosis still relies on clinical assessment, detailed history-taking, and excluding other conditions, all of which take time.
9. Medication side effects (including supplements)
Could something you're taking be making you tired? Beta-blockers for blood pressure or heart conditions, antihistamines, antidepressants, statins, and even some herbal supplements can all cause fatigue as a side effect.
A thorough medication review, including over-the-counter and "natural" remedies, takes time. In a short appointment, it's easy to overlook, especially if the medication was started years ago and you've forgotten it might be relevant.

10. Mental health: depression and anxiety (which are medical, not moral, diagnoses)
Depression doesn't always present as sadness. Sometimes it shows up as overwhelming tiredness, loss of interest, difficulty concentrating, and physical heaviness. Anxiety can be equally exhausting; your nervous system is on high alert all the time.
Exploring mental health properly requires trust, time, and often more than one conversation. A 10-minute slot, especially a first appointment about fatigue, often isn't enough to have that discussion in depth. And there's still stigma; many people worry that if a doctor suggests depression, it means they're not being taken seriously or that the fatigue is "all in their head." It isn't. Depression is a medical condition with real, physical effects.
What happens next?
If you've had normal bloods but still feel dreadful, don't assume you're stuck. The next step is a longer, more detailed consultation with someone who has time to take a full history, review all your symptoms, and think about what hasn't been checked yet.
This might involve:
Repeating some tests with more specific markers
Arranging specialist investigations (sleep studies, autonomic testing, detailed thyroid panels)
Reviewing medications and supplements
Considering referral to relevant specialists (endocrinology, rheumatology, respiratory medicine, immunology)
Fatigue with "normal bloods" is frustrating, but it's not a dead end. It just means the answer lies somewhere beyond what a standard 10-minute appointment and basic blood panel can uncover.
When to seek urgent help
Most causes of chronic fatigue aren't emergencies, but some symptoms need same-day assessment. Contact 999 or attend A&E immediately if you have:
Severe chest pain or difficulty breathing
Sudden weakness, numbness, or difficulty speaking (stroke symptoms)
Confusion or feeling very unwell
Fever with a rash that doesn't fade when you press a glass on it
If your fatigue has come on suddenly (over days rather than weeks), or you've lost a lot of weight without trying, contact your GP urgently, same day if possible.

How Dr Paraiso can help
If you've been told your bloods are normal but you're still exhausted and struggling, a longer consultation with a consultant physician can help join the dots. Dr Hassan Paraiso works across acute hospital medicine and general medicine, and understands the diagnostic process for complex, unexplained symptoms.
During a private consultation, there's time to go through your full history, review previous tests properly, and arrange any further investigations that might be needed, whether that's more detailed blood work, specialist referrals, or imaging. Appointments are available in person in Salford and Greater Manchester, or online anywhere in the UK.
This article provides general information only and is not a substitute for personal medical advice. If you are unwell or worried about a symptom, please speak to a healthcare professional. Call 999 or attend A&E immediately if you have severe chest pain, trouble breathing, signs of stroke, feel very unwell, or think it is an emergency.



Comments